Executive Summary
A leading pharmacy benefits organization set out to enhance how clients analyze and optimize their prescription drug plans. The goal was to create a centralized platform where users could simulate benefit outcomes using real claims data, enabling smarter plan design through dynamic exclusions, rebate strategies, and pricing rules.
Factspan developed a rule-based Admin Portal powered by serverless architecture to automate data ingestion, enrichment, and savings analysis. The platform allowed users to upload claim files, configure benefit parameters, and instantly visualize savings across drug categories, resulting in streamlined workflows and improved plan performance insights.
About the Client
The client operates at the intersection of pharmacy benefits and data analytics, serving a wide network of healthcare stakeholders. With rising drug costs and fragmented decision-making tools, the organization needed a unified portal to drive evidence-based benefit strategies through automation, configurability, and advanced enrichment logic.
Business Challenge
The client faced limitations in analyzing how different plan configurations affected overall savings. Manual claims evaluation, inconsistent field mapping, and lack of simulation capabilities led to missed opportunities for cost control. Users needed the ability to configure exclusions, copays, and rebate models while running automated savings calculations based on historical claims data.
A solution was required that combined intuitive workflows with backend automation, simplifying field mapping, applying enrichment rules, and presenting real-time insights into plan performance and cost-saving opportunities.
Our Solution
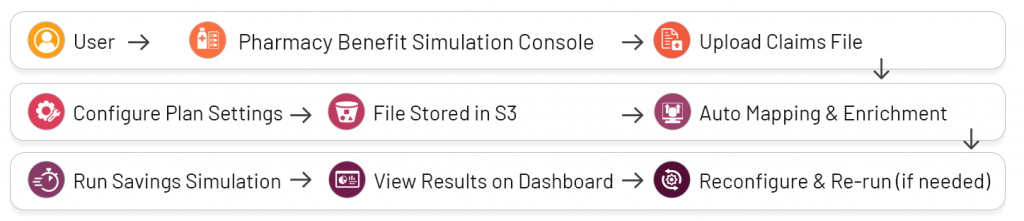
Factspan developed a cloud-native Pharmacy Benefit Simulation Console on AWS to help the client and its users model savings outcomes based on real claims data and configurable benefit parameters.
Claims Ingestion & Mapping:
Users upload claims via the portal, which are stored in S3. Lambda functions auto-map columns using a variations table, with manual override for critical fields.
Simulation Setup:
Users configure parameters such as plan exclusions, formulary rules, copays, DAW penalties, and rebate models. These inputs are saved under an Opportunity ID and used to drive simulations.
Enrichment & Savings Analysis:
Mapped files are enriched using rules for drug classification, age, and channel. Multiple simulations are then triggered across categories like:
- Formulary & Plan Exclusions
- Diabetes & Weight-Loss Impact
- High-Dollar Claims & Prior Auth
- Quantity Limits & Contract Savings
Interactive Reporting:
Users can tweak parameters and instantly rerun simulations. Savings outcomes are visualized in the Clinical Savings section for comparison and optimization.
Architecture:
Built on AWS Lambda, S3, API Gateway, PostgreSQL, and Python, the platform uses a modular, serverless design for scalability, testability, and low overhead.
Our Solution
Business Impact:
- 70% reduction in manual effort for field mapping
- 2x faster claims processing with automated enrichment
- 40% quicker turnaround for savings insights
- 80% increase in plan configuration flexibility
Featured content

